
Back pain is a prevalent condition that can impact individuals of all ages and walks of life. Understanding the various types of back pain can help shed light on the underlying causes and guide appropriate treatment strategies. In this article, we will explore the world of back pain, shining a spotlight on three common conditions that cause discomfort: sciatica, herniated discs, and muscle strains. By taking a closer look at these prevalent culprits, we aim to provide you with a deeper understanding of their effects on your well-being and equip you with valuable insights to effectively manage and alleviate your back pain.
Unraveling Sciatica
What is Sciatica?
Have you ever experienced a shooting pain that starts in your lower back and travels down one of your legs? This excruciating pain might be a symptom of sciatica. Sciatica is not a medical condition itself, but rather a set of symptoms caused by the compression or irritation of the sciatic nerve. Originating from the lower spine, the sciatic nerve is the longest nerve in the human body, extending through the buttocks and down the legs.
What Causes Sciatica?
There are various causes of sciatica, with the most common being a herniated disc. When a disc between the vertebrae bulges or ruptures, it can put pressure on the sciatic nerve, leading to pain and discomfort. Other potential causes include spinal stenosis (narrowing of the spinal canal), bone spurs, degenerative disc disease, and even muscle imbalances or tightness that irritate the nerve.
What are the Symptoms of Sciatica?
The symptoms of sciatica can vary from person to person, but common indicators include:
- A sensation of sharp, shooting pain can be felt originating from the lower back, extending through the buttocks, and traveling down one leg.
- Tingling or a “pins and needles” sensation in the leg or foot.
- Numbness or weakness in the leg or foot.
- Pain that worsens with prolonged sitting, standing, or movement like walking or bending.
- Difficulty controlling the affected leg or foot, sometimes resulting in clumsiness or tripping.
How is Sciatica Diagnosed?
If you suspect you may have sciatica, it’s important to consult a healthcare professional for an accurate diagnosis. Your doctor will likely start the diagnosis by asking about your symptoms and medical history. They may then perform a physical examination, checking for reflexes, muscle strength, and any signs of nerve irritation. Imaging tests such as X-rays, MRI scans, or CT scans might be ordered to identify the underlying cause and assess the severity of the condition.
How is Sciatica Managed and Treated?
The management and treatment of sciatica often depend on the underlying cause and the severity of symptoms. In many cases, non-surgical treatments are effective in relieving pain and promoting healing. These may include:
- Pain medication: Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) or prescription medications can help reduce inflammation and alleviate pain.
- Physical therapy: Targeted exercises and stretches can improve flexibility, strengthen the core and supporting muscles, and relieve pressure on the sciatic nerve.
- Heat and cold therapy: Applying heat packs or ice packs to the affected area can help reduce inflammation and provide temporary pain relief.
- Epidural steroid injections: In more severe cases, corticosteroid injections into the area surrounding the affected nerve may be recommended to reduce inflammation and alleviate pain.
- Surgical intervention: Surgery is typically considered as a last resort when non-surgical treatments fail to provide relief or if there is a severe underlying condition requiring immediate attention.
Understanding Herniated Discs
The Role of Intervertebral Discs
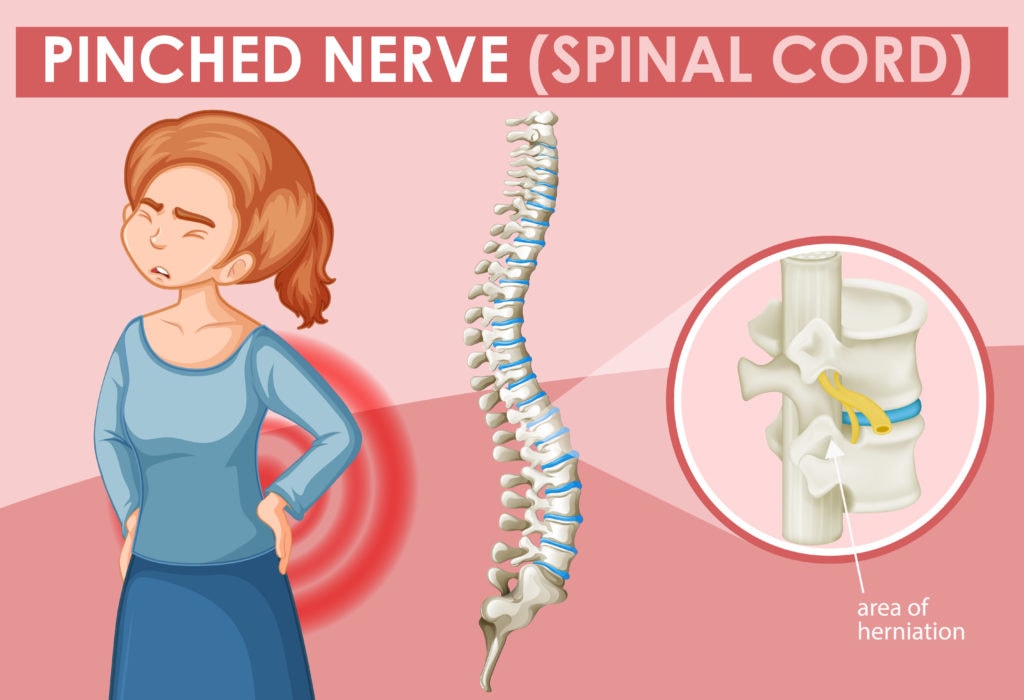
Intervertebral discs act as shock absorbers between the vertebrae, providing cushioning and allowing for spinal flexibility. A herniated disc occurs when the inner gel-like material of a disc protrudes through a weakened or damaged outer layer.
This condition can lead to localized pain, as well as symptoms that radiate to other parts of the body, depending on the location of the affected disc.
The exact causes of herniated discs can vary, but they often occur as a result of age-related degeneration or sudden trauma to the spine. Factors such as repetitive strain, improper lifting techniques, obesity, and genetics can also contribute to the development of herniated discs.
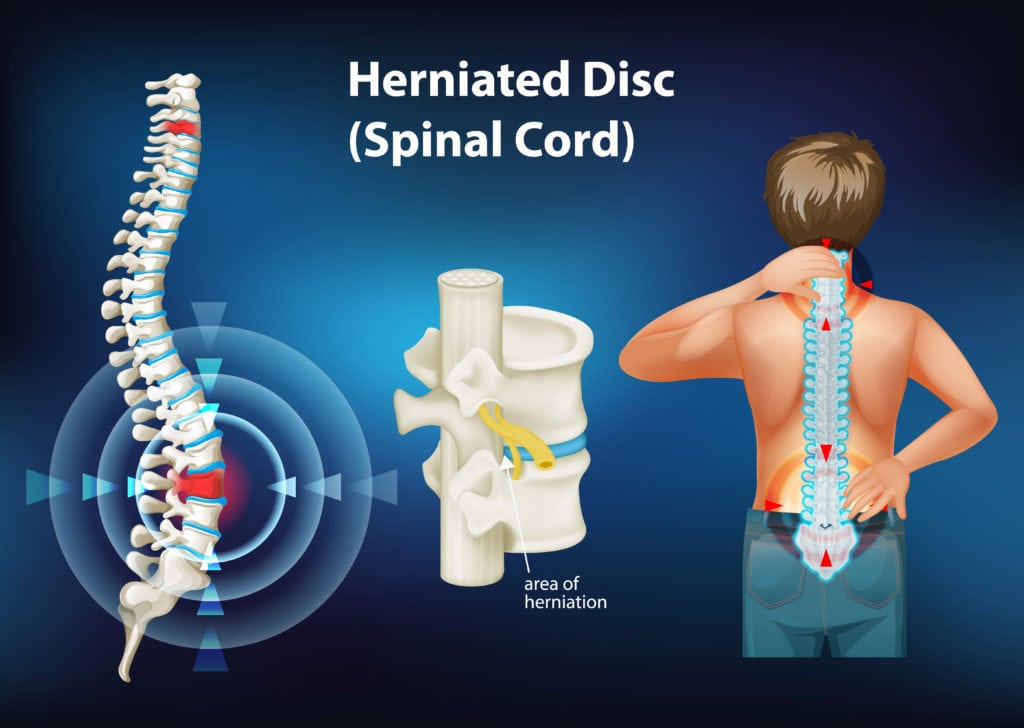
Symptoms and Diagnosis
Herniated discs can cause localized back pain, radiating pain, muscle weakness, and sensory changes. The specific symptoms experienced depend on the location and severity of the herniation. Healthcare professionals diagnose herniated discs through physical examinations, medical history, and imaging tests like MRI or CT scans to visualize the affected area.
Treatment and Rehabilitation
The treatment of herniated discs varies depending on the severity of symptoms. Conservative measures are typically recommended as the initial approach and may include:
- Rest: Taking a break from activities that aggravate symptoms allows the body to heal naturally.
- Physical Therapy: Targeted exercises and stretches can help strengthen the surrounding muscles, improve posture, and alleviate pressure on the affected disc.
- Pain Management: Over-the-counter pain relievers or prescription medications may be recommended to manage discomfort.
- Heat and Cold Therapy: Application of either heat or cold packs to the affected area, which can effectively reduce inflammation and provide temporary relief from pain.
- Epidural Steroid Injections: In some cases, corticosteroid injections may be administered near the affected disc to reduce inflammation and alleviate pain.
- Surgery: Surgical intervention is considered when conservative treatments fail to provide relief or in severe cases. Surgical options may include discectomy, laminectomy, or spinal fusion.
Exploring Muscle Strains
Muscle Strains in the Back
Muscle strains occur when muscle fibers tear due to excessive stretching or overexertion. In the back, strains often affect the muscles supporting the spine, leading to localized pain and limited mobility.
These strains occur when the muscles in the back are stretched beyond their limits or torn due to sudden or excessive force. They can happen during physical activities, lifting heavy objects, or even from simple movements performed with improper form.
The muscles of the back, including the erector spinae, rhomboids, and trapezius, are responsible for supporting the spine and maintaining proper posture. When these muscles experience strain, it can result in localized pain and stiffness in the affected area. The severity of a back muscle strain can range from mild, with minimal tearing of muscle fibers, to severe, involving a complete rupture of the muscle.


Symptoms and Diagnosis
Symptoms of muscle strains in the back include sharp pain, muscle stiffness, and difficulty with certain movements. Healthcare professionals diagnose muscle strains based on physical examinations, medical history, and sometimes imaging tests like X-rays or MRI scans to rule out other potential causes of pain.
Treatment and Rehabilitation
The treatment of muscle strains typically involves a combination of rest, pain management, and rehabilitation techniques:
- Rest: Allowing the injured muscles to rest and recover is crucial for healing.
- Ice or Heat Therapy: Application of either heat or cold packs to the affected area, which can effectively reduce inflammation and provide temporary relief from pain.
- Pain Medication: Over-the-counter pain relievers may be recommended to manage discomfort.
- Physical Therapy: A structured physical therapy program can help restore strength, flexibility, and function to the affected muscles through targeted exercises and stretches.
- Gradual Return to Activity: As the muscles heal, gradually reintroducing physical activity with proper form and technique is essential to prevent re-injury.
Understanding the different types of back pain, including sciatica, herniated discs, and muscle strains, provides valuable insights into the underlying causes and treatment options. By recognizing the symptoms and pursuing appropriate management strategies, individuals can better manage and alleviate their back pain. Remember, consulting with healthcare professionals, following recommended treatment plans, and implementing lifestyle modifications can contribute to improved back health and overall well-being.
